Patent Foramen Ovale (PFO)
Adapted from "Holes in the Heart," Stroke Connection Magazine, January/February 2011
A hole in your heart would seem to be the very definition of a "problem." Yet more than a quarter of the population has one, and for most it causes no adverse health effects. In fact, the vast majority of those affected don't even know it.
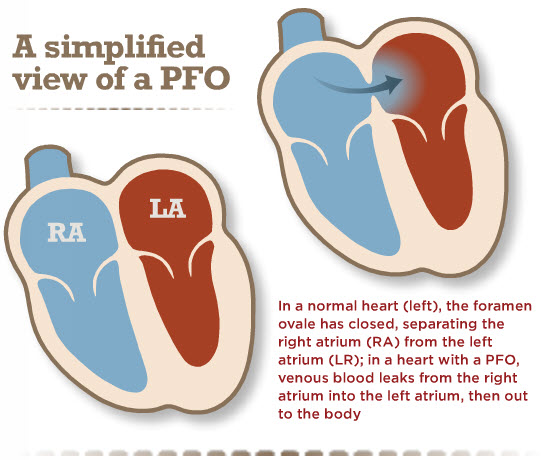
There are two kinds of holes in the heart. One is called an atrial septal defect (ASD), and the other is a patent foramen ovale (PFO). Although both are holes in the wall of tissue (septum) between the left and right upper chambers of the heart (atria), their causes are quite different. An ASD is a failure of the septal tissue to form between the atria, and as such it is considered a congenital heart defect, something that you are born with. Generally an ASD hole is larger than that of a PFO. The larger the hole, the more likely there are to be symptoms.
PFOs, on the other hand, can only occur after birth when the foramen ovale fails to close. The foramen ovale is a hole in the wall between the left and right atria of every human fetus. This hole allows blood to bypass the fetal lungs, which cannot work until they are exposed to air. When a newborn enters the world and takes its first breath, the foramen ovale closes, and within a few months it has sealed completely in about 75 percent of us. When it remains open, it is called a patent foramen ovale, patent meaning open. For the vast majority of the millions of people with a PFO, it is not a problem, even though blood is leaking from the right atrium to the left. Problems can arise when that blood contains a blood clot.
"Blood clots form in our veins all the time," said Dr. David Thaler, associate professor of neurology at Tufts University School of Medicine and director of the Comprehensive Stroke Center at Tufts Medical Center in Boston. "These are tiny blood clots of just a few millimeters that travel from all over the body into the vena cava where they enter the right upper chamber of the heart." From there they are pumped into the right ventricle, from where they enter the lungs. These tiny blood clots (individually called a venous thrombus) get filtered by the tiny capillaries in the lungs, after which the freshly oxygenated blood enters the left atrium, then the left ventricle. From the left ventricle, the blood is pumped out into the miles of blood vessels that feed oxygen and nutrients to every cell in our bodies. "Our lungs normally filter out these tiny clots, but a 2mm thrombus in the brain can cause real havoc," Dr. Thaler said.
That can happen when someone has a PFO or ASD. "PFOs don't actually cause strokes, but they provide a portal through which a thrombus might pass from the right to the left side of the circulation," said Dr. Patrick O'Gara, professor of medicine at Harvard Medical School and executive director of the Shapiro Cardiovascular Center. Depending on whether the clot takes a right or left turn as it exits the heart, it can travel to the brain and cause stroke or TIA. Statistically speaking, the odds of this happening are low, but it can happen.
How would you know?
Finding out whether you have a PFO is not easy, and it's something that isn't usually investigated unless a patient is having symptoms like severe migraines, TIA or stroke. Although the prevalence of PFO is about 25 percent in the general population, this increases to about 40 to 50 percent in patients who have stroke of unknown cause, referred to as cryptogenic stroke. This is especially true in patients who have had a stroke before age 55. In some cases, the PFO combines with another condition, such as atrial fibrillation, to increase the risk of stroke.
For survivors who don't have a definitive cause of their stroke, Dr. O'Gara suggests meeting with their neurologist to discuss the possibility of PFO. "There are many causes of stroke and having a PFO accounts for only a very small number," Dr. O'Gara said. PFO is diagnosed with an echocardiogram. An echocardiogram, also called a cardiac echo, creates an image of the heart using ultrasound.
What's to be done?
"The greatest myth about PFOs is that they must be closed. The vast majority of them require no treatment," Dr. O'Gara said. "If someone has one that is related to symptoms, they can be treated with aspirin, warfarin or catheter closure, depending on the circumstances."
Of course, drugs don't close the hole, "so the aim of drug treatment is to prevent a clot from forming in the first place," Dr. Thaler said. Nothing will close it except open-heart surgery or a closure device placed by a catheter threaded from the groin through the veins to the heart. Until recently, there were no approved catheter-closure devices designed for PFOs. The FDA has approved a device for patients who've had a stroke believed to be caused by a PFO, which reduces the risk of another stroke.