Pulmonary Hypertension - High Blood Pressure in the Heart-to-Lung System
What is pulmonary hypertension?
Pulmonary hypertension (PHT) is high blood pressure in the heart-to-lung system that delivers fresh (oxygenated) blood to the heart while returning used (oxygen-depleted) blood back to the lungs.
Pulmonary versus systemic blood pressure
Unlike systemic blood pressure, which represents the force of your blood moving through the blood vessels in your body, pulmonary blood pressure reflects the pressure the heart exerts to pump blood from the heart through the arteries of the lungs. In other words, it focuses on the pressure of the blood flow in your lungs.
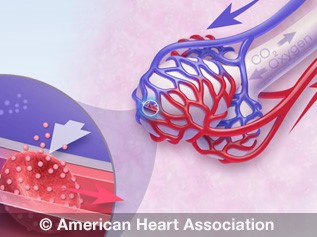
How blood flows through your heart and lungs
The lower right heart chamber, the right ventricle, receives oxygen-depleted blood and pumps it to your pulmonary arteries. The blood then travels to your lungs to be oxygenated, and on to the upper left heart chamber, the left atrium. From there, the oxygen-rich blood moves into the lower left chamber, the left ventricle, which pumps blood to the rest of your body through the aorta.
Watch how blood flows through your heart and lungs.
The numbers in pulmonary hypertension
Pulmonary blood pressure is normally a lot lower than systemic blood pressure. Normal pulmonary artery pressure is 8-20 mm Hg at rest. If the pressure in the pulmonary artery is greater than 25 mm Hg at rest or 30 mmHg during physical activity, it is abnormally high and is called pulmonary hypertension.
The long-term effects of pulmonary hypertension
Similar to how systemic high blood pressure can cause the heart to work harder to deliver blood to the body, pulmonary hypertension can occur when the arteries in the lungs narrow and thicken, slowing the flow of blood through the pulmonary arteries to the lungs. As a result, the pressure in your arteries rises as your heart works harder to try to force the blood through. Heart failure occurs when the heart becomes too weak to pump enough blood to the lungs.
Symptoms of pulmonary hypertension
Early symptoms include:
- Shortness of breath during routine activity
- Fatigue
- Chest pain
- Racing heartbeat
- Pain in upper right side of abdomen
- Decreased appetite
Later symptoms include:
- Feeling light-headed, especially during physical activity
- Fainting
- Swelling in the ankles or legs
- Bluish lips or skin
Diagnosis and treatment
Pulmonary hypertension can develop slowly, without early signs and symptoms. When symptoms do occur, they may be attributed to asthma or other lung or heart conditions.
To diagnose pulmonary hypertension, your doctor may ask about your symptoms and risk factors, including other medical conditions and family history. Having a family member with pulmonary hypertension increases your risk of developing the disease.
Medical evaluation
Your physician may recommend tests and procedures to diagnose pulmonary hypertension and discover its cause and severity. Common diagnostic tests include an echocardiograph, chest X-ray, electrocardiogram (EKG) and catheterization of the right heart. Discovering the underlying cause may involve a chest CT scan, chest MRI, lung function tests, polysomnogram (PSG), lung ventilation/perfusion scan and blood tests.
Once you have a diagnosis of pulmonary hypertension, exercise testing can help your doctor determine its severity. The test measures how well your heart and lungs work while you are on a treadmill or bicycle, so the doctor can rate your activity level. Exercise testing may be ongoing during your treatment in order to monitor your progress.
Types of pulmonary hypertension
The World Health Organization has established five groups of pulmonary hypertension.
Group 1 pulmonary arterial hypertension (PAH)
Group 1 PAH includes pulmonary hypertension that has no known cause; is inherited; is caused by drugs or toxins; is caused by conditions such as connective tissue disease, HIV infection, liver disease, congenital heart disease, sickle cell disease, or schistosomiasis; or is caused by conditions that affect the veins and small blood vessels of the lungs.
Group 2 pulmonary hypertension
Group 2 pulmonary hypertension is often associated with left heart disease such as mitral valve disease or long-term high blood pressure. Left heart disease is the most common cause of pulmonary hypertension.
Group 3 pulmonary hypertension
Group 3 is related to lung problems like chronic obstructive pulmonary disease (COPD) and interstitial lung disease, as well as sleep apnea and other sleep-related breathing disorders.
Group 4 pulmonary hypertension
Group 4 includes pulmonary hypertension caused by blood clots in the lungs or general clotting disorders.
Group 5 pulmonary hypertension
Group 5 includes pulmonary hypertension triggered by other disorders. Examples of such diseases or conditions are blood disorders such as polycythemia vera and essential thrombocythemia; systemic disorders such as sarcoidosis and vasculitis; metabolic disorders such as thyroid and glycogen storage disease; and other conditions such as kidney disease and tumors that press on the pulmonary arteries.
Factors that can affect pulmonary hypertension
While pulmonary hypertension has no cure, you can live an active, fulfilling life by working with your doctor to manage your symptoms. Talk to your doctor before taking over-the-counter medicine, as some can worsen symptoms of pulmonary hypertension or interfere with prescriptions — and keep a list of medicines with you. Ask whether you should get a pneumonia vaccination or flu shot. Additionally, pregnancy can pose serious risks for women with pulmonary hypertension, so be sure to discuss birth control options with your physician.
These lifestyle changes can improve your symptoms:
- Quit smoking. Your doctor can recommend programs and products to help.
- Follow a healthy diet. Eat a variety of fruits, vegetables, and whole grains, plus lean meat, poultry, fish and low-fat/fat-free milk. Your diet should be low in fat, cholesterol, sodium and sugar.
- Watch your weight. A daily record of your weight can help you be aware of rapid weight gain, which may be a sign that your pulmonary hypertension is worsening.
- Stay active. Incorporate physical activity such as walking into your lifestyle. Discuss the level of activity with your doctor. Avoid straining or lifting heavy weights. Rest when you need to.
- Avoid sitting in a hot tub or sauna, or taking long baths, which will lower your blood pressure.
- Be cautious about air travel or high-altitude locales. You may need to travel with extra oxygen.
- Get support for the anxiety and stress of living with pulmonary hypertension. Talk with your health care team, or ask for a referral to a counselor. A support group for people living with pulmonary hypertension can be invaluable in learning how to cope with the illness.