Tetralogy of Fallot
What is it?
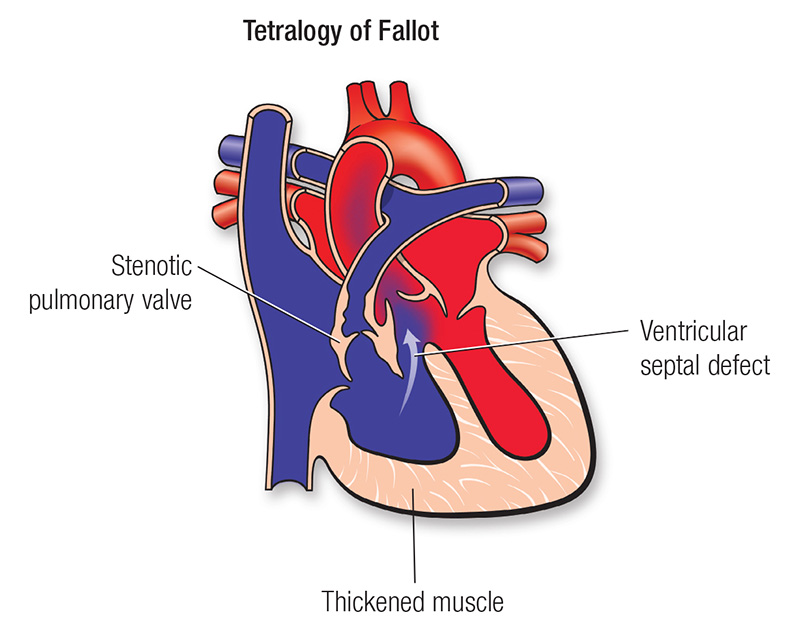
A heart defect that features four problems:
- a hole between the lower chambers of the heart
- an obstruction from the heart to the lungs
- The aorta (blood vessel) lies over the hole in the lower chambers
- The muscle surrounding the lower right chamber becomes overly thickened
More information for parents of children with Tetralogy of Fallot
What causes it?
In most children, the cause of tetralogy of Fallot isn't known. It's a common type of heart defect. It may be seen more commonly in children with Down syndrome or DiGeorge syndrome. Some children can have other heart defects along with tetralogy of Fallot.
How does it affect the heart?
Normally the left side of the heart only pumps blood to the body, and the heart's right side only pumps blood to the lungs. In a child with tetralogy of Fallot, blood can travel across the hole (VSD) from the right pumping chamber (right ventricle) to the left pumping chamber (left ventricle) and out into the body artery (aorta). Obstruction in the pulmonary valve leading from the right ventricle to the lung artery prevents the normal amount of blood from being pumped to the lungs. Sometimes the pulmonary valve is completely obstructed (pulmonary atresia).
How does tetralogy of Fallot affect my child?
Infants and young children with unrepaired tetralogy of Fallot are often blue (cyanotic). The reason is that some oxygen-poor blood is pumped to the body through the hole in the wall between the right and left ventricle instead of being pumped to the lungs.
What can be done about tetralogy of Fallot?
Tetralogy of Fallot is treated surgically. A temporary procedure may be done at first if the baby is small or if there are other problems. Complete repair comes later. Sometimes the first operation is a complete repair.

Temporary Operation
In some infants, a shunt operation may be done first to provide adequate blood flow to the lungs. This isn't open-heart surgery and doesn't fix the inside of the heart. The shunt is usually a small tube of synthetic material sewn between a body artery (or the aorta) and the pulmonary artery. The shunt is closed when a complete repair is done later. Alternatively, a metal stent can be placed in the ductus arteriosus to provide extra blood flow to the lungs. The ductus arteriosus is a fetal blood vessel connecting the aorta to the pulmonary artery. This vessel will normally close by itself over the first day of life but can be kept open with the stent procedure.
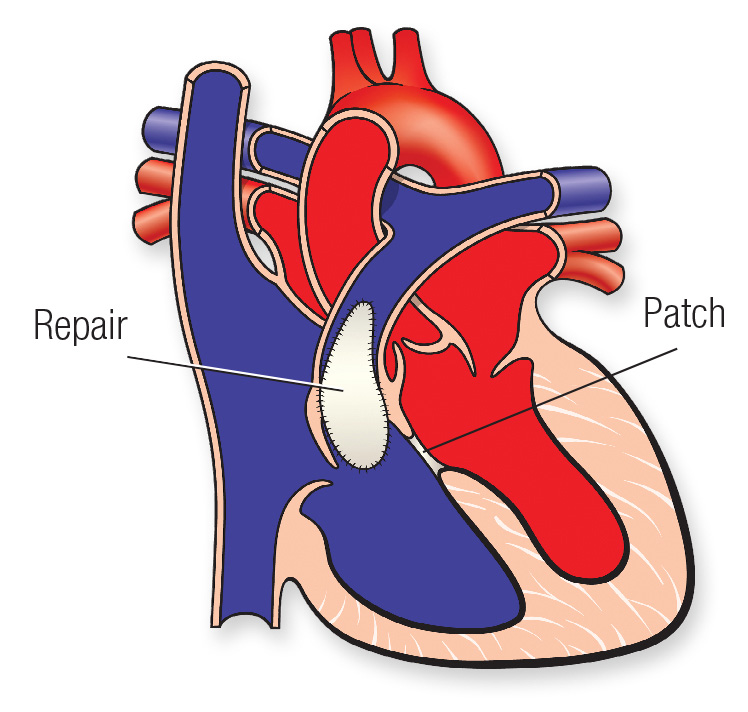
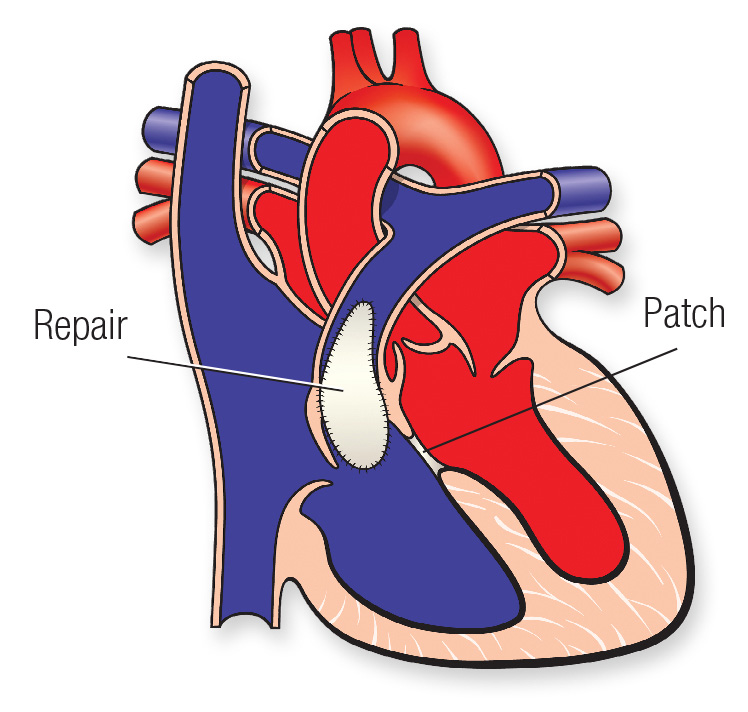
Complete Repair
Complete repair tends to be done early in life. The surgeon closes the ventricular septal defect with a patch and opens the right ventricular outflow tract by removing some thickened muscle below the pulmonary valve, repairing or removing the obstructed pulmonary valve and, if needed, enlarging the branch pulmonary arteries that go to each lung.
Sometimes a tube is placed between the right ventricle and the pulmonary artery. This is sometimes called a Rastelli repair. It's similar to the type of repair used for some other heart defects.
Will my child's activities be limited?
Your child may need to limit physical activity, particularly for competitive sports, if there is leftover obstruction or leak in the pulmonary valve, which is common after repair. Children with decreased heart function or rhythm disturbances may need to limit their activity more.
If the tetralogy has been repaired with surgery, and there's no obstruction or leak in the pulmonary valve, your child may be able to participate in normal activities without much increased risk.
Your child's pediatric cardiologist will help decide if your child needs limits on physical activity.
What will my child need in the future?
If your child has had tetralogy of Fallot repaired, he or she will need regular follow-up with a pediatric cardiologist. As an adult, your child will need lifelong regular follow-up with a cardiologist who's had special training in congenital heart defects.
Some long-term problems can include leftover or worsening obstruction between the right pumping chamber and the lung arteries. Children with repaired tetralogy of Fallot have a higher risk of heart rhythm disturbances called arrhythmias. Sometimes these may cause dizziness or fainting.
Generally, the long-term outlook is good, but some children may need medicines, heart catheterization or even more surgery.
What about preventing endocarditis?
Children with tetralogy of Fallot are at increased risk for endocarditis. Some children, including those have had a valve replacement, still have a shunt or have leaks around surgical patches, and need to take antibiotics before certain dental procedures to help prevent endocarditis. See the section on Endocarditis for more information.
Congenital Heart Defect ID sheet
More information for adults with Tetralogy of Fallot
What causes it?
In most cases, the cause isn't known although in some patients, genetic factors play a role. It's a common type of heart defect. It may be seen more commonly in patients with Down syndrome (in association with AV canal defects) or DiGeorge syndrome. Some patients can have other heart defects along with tetralogy of Fallot.
How does it affect the heart?
Normally the left side of the heart only pumps blood to the body, and the heart's right side only pumps blood to the lungs. In a patient with tetralogy of Fallot, blood can travel across the hole (VSD) from the right pumping chamber (right ventricle) to the left pumping chamber (left ventricle) and out into the body artery (aorta). Obstruction in the pulmonary valve leading from the right ventricle to the lung artery prevents the normal amount of blood from being pumped to the lungs. Sometimes the pulmonary valve is completely obstructed (pulmonary atresia).
How does tetralogy of Fallot affect me?
Most patients are diagnosed with tetralogy of Fallot as infants or young children. Patients with unrepaired tetralogy of Fallot are usually blue (cyanotic). This is true in infants, children and adults with unrepaired tetralogy of Fallot. Most adults with tetralogy of Fallot have had it repaired in childhood. Many people are symptom free but may have residual or recurrent problems. These include valve leakage of blood into the heart's right side, blockage of blood leaving the heart's right side and heart rhythm problems. Some patients with these problems may have limited exercise tolerance and may require medicines, repeat operations and/or a special pacemaker to lower the risk of heart rhythm problems.
What can be done about tetralogy of Fallot?
Tetralogy of Fallot is treated with two kinds of surgery. One provides temporary improvement by a shunt to give more blood flow to the lungs. The other is a complete repair of the two most important abnormalities that make up tetralogy of Fallot. Patients might have one or both surgeries in their lifetime.

Shunt Operation
In some patients, a shunt operation may be done first to provide more blood flow to the lungs. This is not open-heart surgery and doesn't fix the inside of the heart. The shunt is usually a small tube of synthetic material sewn between a body artery (or the aorta) and the pulmonary artery. The shunt is removed when a complete intracardiac repair is done later. This is usually done in babies to allow them grow big enough to have a full repair but is occasionally done in adults if a complete repair isn't an immediate option. Some adults had shunts as children, but never got a complete repair. Those patients may still be able to get a complete repair, even as adults.
Complete Repair
Complete repair tends to be done early in life, but in some cases it can be done in adulthood. The surgeon closes the ventricular septal defect with a patch and relieves the obstruction to blood flow going to the lungs. This may be done by removing some thickened muscle below the pulmonary valve, repairing or removing the obstructed pulmonary valve and, if needed, enlarging the pulmonary artery branches that go to each lung. Sometimes a tube (conduit) with a valve in it is placed between the right ventricle and the pulmonary artery. This is sometimes called a Rastelli repair. It's similar to the type of repair used for some other heart defects.
Repeat Operations
The surgery to open up the pulmonary valve often leads to a leaky pulmonary valve. Although this is better tolerated than the original abnormality, the leaky valve can eventually cause problems. There also can be obstructed pathways that are left behind or develop as the patient grows. Both leaky valves and obstructed pathways can cause problems for adult patients with tetralogy of Fallot. In many cases, another surgery to replace the pulmonary valve may be needed in adolescence or adulthood.
Ongoing Care
Medical
If you've had tetralogy of Fallot repaired, you'll need regular follow-up with a cardiologist who's had special training in congenital heart defects. You may need to take medicine before or after your operation to help your heart muscle contract or to control heart rhythm abnormalities. Your cardiologist will follow your progress with various tests. These include electrocardiograms, Holter monitors, exercise stress tests, echocardiograms and cardiac MRIs. This will help determine if you need another procedure, such as a cardiac catheterization or more surgery. You should also consult a cardiologist with expertise in caring for adults with congenital heart disease if you're undergoing any type of non-heart surgery or invasive procedure.
Activity Restrictions
If tetralogy of Fallot has been repaired with surgery, and there's no obstruction or leak in the pulmonary valve, you may be able to participate in normal activities without much increased risk. You may need to limit your activity if there is leftover obstruction or a pulmonary valve leak, which is common after repair. This limitation may be especially necessary for competitive sports. Patients with decreased heart function or rhythm abnormalities may need to limit their activity more. Your cardiologist will help decide if you need limits. See the Physical Activity section for more information.
What will I need in the future?
If you've had tetralogy of Fallot repaired, you'll need regular lifelong regular follow-up with a cardiologist who's had special training in congenital heart defects.
Some long-term problems can include leftover or worsening obstruction between the right pumping chamber and the lung arteries. Another problem can be a leaky pulmonary valve and enlargement of the heart's right side. Patients with repaired tetralogy of Fallot have a higher risk of heart rhythm disturbances called arrhythmias. Sometimes these may cause dizziness or fainting.
Generally, the long-term outlook is good, but some patients may need medicines, heart catheterization or even more surgery.
Endocarditis Prevention
People with tetralogy of Fallot are at increased risk for developing endocarditis. People with unrepaired and partially repaired tetralogy will need antibiotics to prevent endocarditis before certain dental procedures. If your tetralogy of Fallot has been repaired, your cardiologist will let you know if you need to continue to receive these routine antibiotics. See the section on Endocarditis for more information.
Problems You May Have
Heart Function
In the long-term postoperative period, your heart muscle function may decrease and you'll need medication. This usually reflects weakening function of the right side of the heart, but in rare instances decreased function of the left ventricle may also occur. Medicines that may be needed include diuretics (water pills), drugs to help your heart pump better and drugs to control your blood pressure.
Heart Rhythm Disturbances
People with repaired tetralogy of Fallot have a higher risk of heart rhythm disturbances called arrhythmias. These can originate from the atria or the ventricles. Sometimes they may cause dizziness or fainting. You may need medicine to control them. Sometimes patients also need *blood thinners to reduce the risk of stroke related to the arrhythmias. In rare cases, you may need a procedure in the cardiac catheterization laboratory or the operating room to eliminate these arrhythmias and control symptoms. See the Arrhythmias section for more information. Some patients need pacemakers or implantable defibrillators to treat their arrhythmias.
Pregnancy
In many cases, women with repaired tetralogy of Fallot have successful, full-term pregnancies. Some woman with significant residual heart problems may be at risk for a difficult pregnancy. See the section on Pregnancy for more information. Once tetralogy of Fallot has been repaired, the pregnancy risk is low unless the woman has some side effects or residual effect like irregular heart rhythms or persistent narrowing of the pulmonary valve. Any woman considering pregnancy should have a complete physical examination by her cardiologist in consultation with a multi-disciplinary team before becoming pregnant to find out what, if any risk there might be with the pregnancy. Pregnancy is considered to be high-risk and not recommended for women with unoperated tetralogy of Fallot who remain "cyanotic" (blue).
Will I need more surgery?
After the first complete repair, residual problems may require you to have more open-heart surgeries or procedures in the cardiac catheterization laboratory. In some cases, a procedure done in the cardiac catheterization laboratory using a balloon-tipped catheter to dilate and/or place an expandable stent in narrowed areas may be needed.







